
23 Apr Ten Years After Ebola: Learnings for Lassa Fever, “Lassa-X” and Pandemic Preparedness Lead
2014 Ebola epidemic in West Africa serves as a stark reminder of the vulnerabilities and strengths of public health systems. As the world continues to face emerging and re-emerging infectious diseases, the lessons from the Ebola crisis remain as relevant 10 years later.
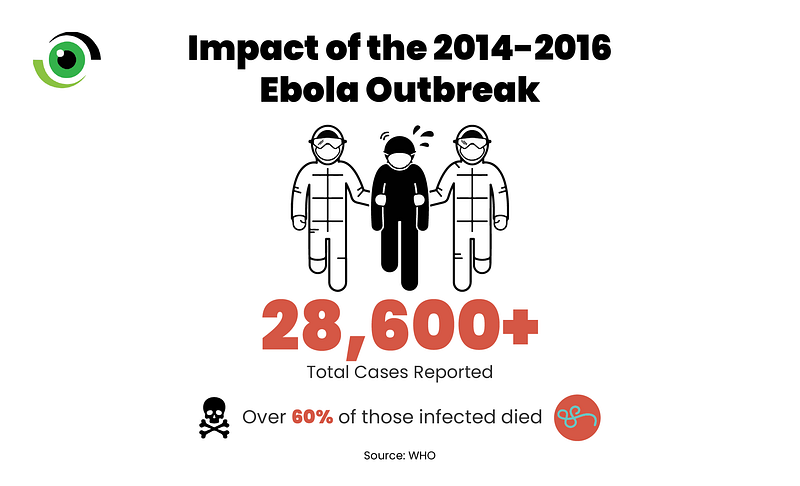
The 2014 Ebola epidemic, which primarily impacted Guinea, Sierra Leone and Liberia, was the largest and most complex outbreak of the virus since its discovery in 1976. The initial slow response and lack of coordination among agencies compounded the crisis, enabling the virus to spread uncontrolled across borders and what started as a regional health crisis, rapidly escalated into a global emergency. By the time the World Health Organization (WHO) declared the outbreak over in 2016, more than 28,600 cases had been reported, with more than 60% (11,325) of deaths. In the hardest-hit countries, healthcare systems collapsed under the pressure, resulting in an increase in mortality from other diseases such as malaria, tuberculosis, and HIV/AIDS owing to a lack of access to medical care.
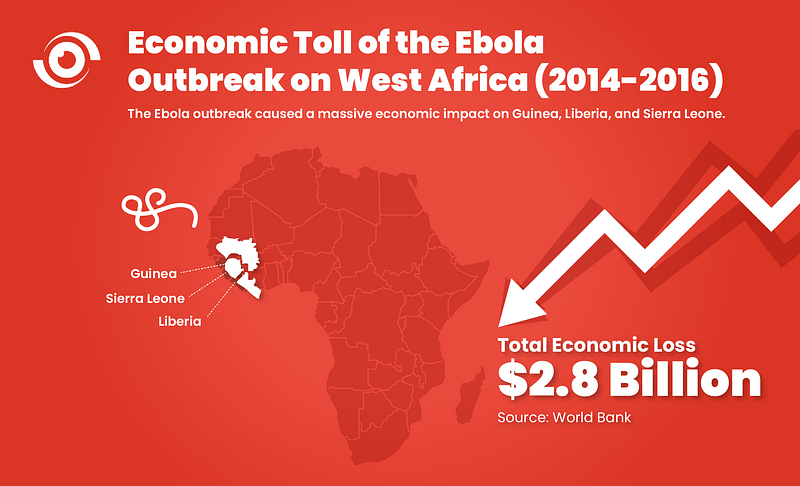
Apart from the destructive effects on health systems, the 2014 Ebola epidemic devastated economies. According to the World Bank, the overall impact of Ebola was estimated at $2.8 billion in the three hardest-hit countries, with a per capita Gross Domestic Product drop averaging $125 across the three nations. Severe shocks to investment, production, and consumption, coupled with a 30–60% drop in bauxite, iron ore, and gold prices, compounded the economic damage. Furthermore, the epidemic inceased unemployment, decreased incomes, and disrupted education. While foreign aid helped cushion fiscal deficits, the economic recovery has been gradual. The epidemic demonstrated to the world how a regional outbreak could have far-reaching consequences.
The next pandemic — the hypothetical threat of Lassa-X and precedent of learning from the past
West Africa is no stranger to viral haemorrhagic fevers (VHFs) such as Ebola, with Lassa fever being another health concern that is endemic in the region. Lassa fever, which is endemic in countries such as Nigeria, Liberia and Sierra Leone amongst others, is a VHF that is quite similar to Ebola. While Lassa fever has a lower fatality rate, its endemic nature and the difficulties of early detection make it a persistent threat in the region. Healthcare workers are especially vulnerable, since the disease can be mistaken for common conditions like malaria or obstetric emergencies, resulting in high transmission rates in hospital settings, where the index of suspicion may be low. The rapid spread of VHFs, as shown during the 2014 Ebola crisis, demonstrates how quickly a localised outbreak can escalate into a global emergency. Similarly, Lassa fever can spread quickly , in densely populated and high-mobility areas.
A recent study funded by the Coalition for Epidemic Preparedness Innovations (CEPI) modelled “Lassa-X,” a hypothetical Lassa-related virus with higher transmissibility and virulence, to assess vaccination strategies within the 100 Days Mission. Over the next ten years, Lassa fever is expected to cause 237,000 hospitalisations, 39,000 deaths, and the value of statistical life (VSL) lost, estimated at $15.3 billion. The study found that population-wide preventive vaccination campaigns, though requiring more vaccine doses, offered greater health-economic benefits than reactive strategies. If a vaccine 70% effective against disease were administered to 40% of the population within 100 days, it could save 5,500 lives and prevent 33,300 hospitalisations within a two-year period.
Top three takeaways from the 2014 Ebola epidemic and its implications for Lassa and Lassa-X
1. Enhancing Surveillance Systems for Rapid Epidemic Response
The 2014–2016 Ebola epidemic revealed the consequences of poor surveillance, slow data sharing and delayed response, enabling Ebola to rapidly spread across West Africa, with early cases being undetected and unreported. For example, it took about three months to diagnose Ebola in Guinea, during which time it spread to Liberia and Sierra Leone before it was reported to WHO.
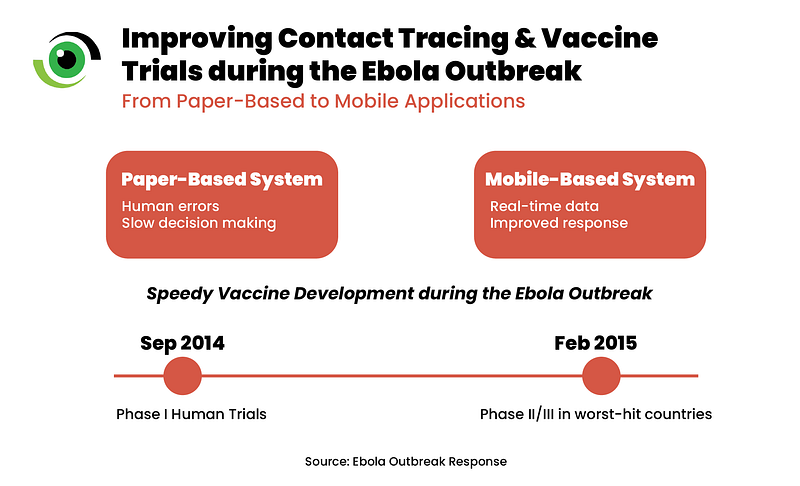
Once the severity of the situation was understood, efforts intensified, and advanced surveillance systems were implemented. Initial paper-based contact tracing was prone to errors, delayed rapid response and decision making. To address this, mobile applications for real-time data reporting were deployed, reducing the time between data entry and use while improving contract tracing and data management. This improved data completeness, storage and accuracy and access to surveillance data for informed response.
The epidemic emphasised the role of centralised leadership in ensuring diverse stakeholders, including non-governmental organisations (NGOs) and international partners, work together for effective surveillance and response systems that are tailored to local needs. However, the absence of cohesive coordination at the initial stage of the epidemic delayed response, exacerbating the spread. While Lassa surveillance remains suboptimal in the most affected countries, initiatives such as the ENABLE study are contributing to a better understanding of Lassa fever’s epidemiology by strengthening surveillance systems, enhancing data sharing, and encouraging collaboration among stakeholders.
2. Accelerating Vaccine Development for Outbreak Control
The rapid research response to the 2014–2016 Ebola outbreak was characterised by the development of a combination of medical countermeasure and the rapid mobilisation of cross-sector partnerships. The global health community worked tirelessly in accelerating the development of an Ebola virus vaccine. In under five months, phase I trials in humans began in September 2014, and by February 2015, phase II and phase III trials had been initiated in all the three worst-hit countries. One trial, using a lab-made virus with Ebola-like proteins, demonstrated vaccine efficacy. This was achieved using a mobile ring vaccination trial, modelled after the strategy that helped eradicate smallpox and targeted new outbreak hotspots. Considering that clinical trials began after the epidemic’s peak, the impact of vaccine interventions on controlling the epidemic may have been limited.
The vaccine development during the epidemic unequivocally showed that the global research community can improve its capacity to implement trials more rapidly and efficiently in outbreaks. This year was the first time a Lassa vaccine candidate entered Phase 2a trials, signifying progress in Lassa vaccine development and emphasising the need for sustained investments to accelerate vaccine development.
3. Building Trust Through Transparent Communication and Community Involvement
The unprecedented scale of the epidemic, combined with the slow and fragmented global response, underscored the importance of involving local communities early and effectively in outbreak management. Community resistance to public health interventions, driven by past experiences and distrust in external parties was a significant barrier to response efforts. In Guinea, this distrust led to violence against outbreak responders, emphasising the need for effective community engagement.
Despite these challenges, there were notable successes. In Sierra Leone, the Community Led Ebola Action (CLEA) approach, which involved local mobilisers and religious leaders effectively engaged communities. This approach resulted in the creation of action plans and real-time monitoring, which led to more safe burials and prompt medical referrals. In Guinea, Liberia and Sierra Leone, the successful implementation of phase II/III Ebola vaccine trials were largely attributed to community acceptance and robust community partnerships. These partnerships were built through transparent communication and the active participation of community leaders.

To develop community trust and collaboration in future outbreaks, strategies include involving community leaders in planning and response, addressing community concerns openly, and providing culturally sensitive education. Strengthening national and subnational leadership and collaboration ensures that responses are well coordinated and locally adapted, enhancing overall effectiveness and resilience to future health emergencies. Community mobilisation and risk communication are being deployed to enhance Lassa fever prevention and response.
The road ahead — Ensuring preparedness for future outbreaks.
Since the Ebola epidemic, global health preparedness has advanced significantly, with improved surveillance systems, rapid response frameworks, and vaccine research and development. However, future outbreaks will require relentless commitment to continuous learning, adaptation, and investment. It is important to highlight resilience, especially when dealing with diseases like Lassa fever. Strengthening multisectoral collaboration and advancing research will be crtical in mitigating risks and enabling timely, effective responses to emerging threats. The road ahead demands continued focus on these priorities to safeguard global health security.



A WordPress Commenter
Posted at 10:34h, 23 AprilHi, this is a comment.
To get started with moderating, editing, and deleting comments, please visit the Comments screen in the dashboard.
Commenter avatars come from Gravatar.